Precisely engineering the genome of human cells remains largely in the realm of science fiction. It's possible, with the right virus, to get new or modified genes into cells. But the regular collection of the genes in the cell are still there—we can't typically eliminate a gene that has gone bad or replace a broken copy with a working one. Although some progress has been made in creating proteins that target specific spots in the genome, it's tough to make these proteins both specific enough to only target a single sequence yet flexible enough to work on lots of targets.
Now, it turns out we don't have to make proteins after all. Bacteria have a system that targets the DNA of viral invaders, acting a bit like an immune system. And two teams of researchers have shown it's possible to direct that system so it targets specific locations in a mammalian genome. Once targeted, the cell's normal DNA repair system can replace the sequence with an engineered one of the researchers' choosing.
The efficiency is under 10 percent, so don't start thinking we're going to edit every cell of the human body. But that rate still makes it practical for a variety of purposes—and potentially even therapies.
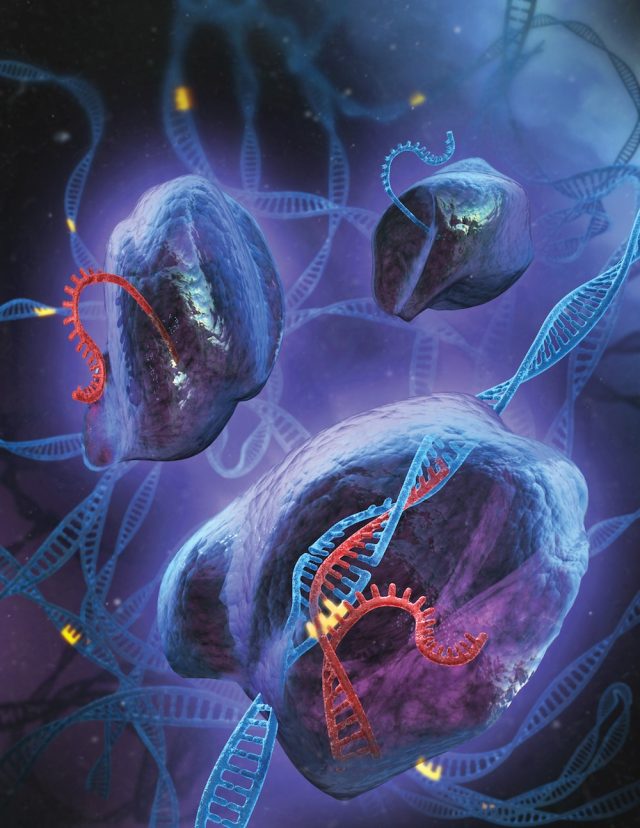
Most people don't think of bacteria as having an immune system. In the sense of our immune system (with its specialized cells and antibodies), they don't. But that doesn't mean they're helpless in the face of invaders. When a DNA-based virus invades, specialized enzymes chop it into small pieces and then insert it into a special area of the bacterial genome. There it's flanked by special tagging sequences. The fragment of DNA and its tags then get turned into RNA that partially matches the sequence of the viral DNA.
A specialized enzyme recognizes the RNA tags and uses the matching bit of sequences to guide it to the DNA of the viral invader. It then makes a cut in the viral DNA, inactivating it. Collectively, this collection of DNA and proteins is called the CRISPR system, and it helps protect bacteria from invasion.
Two teams of researchers reasoned that, in the end, DNA is DNA. If the system worked in bacteria, there was no obvious reason it couldn't also target DNA in mammalian cells. They modified the coding sequence of the enzyme that does the cutting so it works in mammals, then set about designing RNAs that could target sequences in mammalian genomes.
The teams did several demonstrations, but the simplest one to follow is a case where they used a version of the gene that encodes Green Fluorescent Protein (GFP). First, they created a version of the GFP gene that has a mutations in it that keeps it from making a working protein. Without using the CRISPR system, they inserted this defective GFP gene randomly in the genome. Then they designed a guide RNA that includes the CRISPR tags and a sequence that matches the mutant GFP gene.
If they just put the guide RNA and the CRISPR gene that cuts DNA into the cells, it simply cut the genome at the site of the mutation; the cell would then repair the break, often by linking in a completely unrelated section of DNA. If, however, they put a normal, unmutated version of the GFP gene in at the same time, the cell would repair the CRISPR-generated break using this normal copy. The mutation would be eliminated and the cells would start glowing green.
It all worked nicely. The teams used different forms of guide RNAs to damage or repair various genes and even create small deletions. In one case, they modified two ones at the same time. The CRISPR protein that cuts DNA uses separate binding sites to grab each of the two stands of the double helix when making a cut. Mutating one of these sites meant the system would only cut a single strand, creating a nick in the DNA that was more likely to be repaired cleanly. The percentages of success weren't especially high—usually in the area of about five percent—but that will typically mean hundreds of engineered cells in a single culture dish.
Immediately, this will be useful for biologists. Researchers love to study what gene products do inside of cells, often by testing mutations that alter their function. It's easy to replace a gene in bacteria, but it hasn't been easy to do so in mammalian cells. Typically, researchers were left testing mutant genes that expressed far more protein than a cell would normally contain, all with the cell's normal version around confusing the results. This technique would seem to make engineering mammalian cells much more convenient.
Longer term, one of the papers goes as far as suggesting therapeutic applications. This won't be a cure for most genetic diseases in its current form, since the frequency of success means only a few of the target cells will end up being fixed. Still, for some disorders (mostly those involving missing enzymes), even a handful of cells can be enough to provide a fix. With time and experience, it might be possible to get the frequency of CRISPR-mediated repair up to higher levels.
Science, 2013. DOI: 10.1126/science.1232033, 10.1126/science.1231143 (About DOIs).
reader comments
28