When most people think of the nervous system, they think of it as a hub of activity. Sensations trigger nerves, which activate the ones they're connected to, eventually producing a response. What's often overlooked is the fact that shutting nerves down is just as important. Entire classes of nerves exist solely to tell their neighbors to quiet down, while Parkinson's disease is caused by the failure of a circuit that ultimately helps shut down muscle activity.
Another disease that's caused by excessive nerve activity is epilepsy, where the aberrant activation of nerves causes seizures. Researchers decided to try reversing this effect by adding additional inhibitory neurons, derived from embryonic cells, to specific regions of the brains of epileptic mice. The approach worked, which means their next step will probably involve trying to do the same thing with neurons derived from stem cells.
Although epilepsy is a complicated disease in humans, it's possible to model it in mice using a drug called pilocarpine, which activates receptors for the neurotransmitter acetylcholine. Used appropriately, pilocarpine is a valuable drug. But when given systemically (for example, injected into the blood stream), the drug enters the brain and causes excessive neural activity. This can result in long-term changes to the architecture of many neurons in the brain, creating a variety of symptoms that may include seizures, hyperactivity, and altered spatial memory.
To test their epilepsy treatment, the researchers injected mice with pilocarpine and monitored them around the clock for several days. Those that experienced a seizure were used for the study.
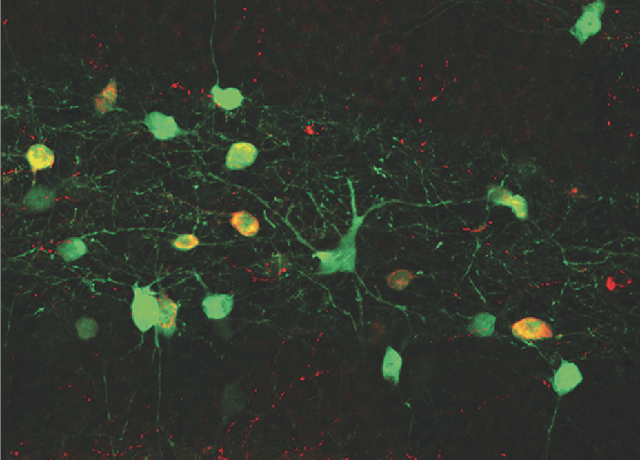
A number of inhibitory neuron types have been identified, but the authors were specifically interested in GABA-producing interneurons of the brain (GABA is an inhibitory neurotransmitter, and an interneuron is a nerve cell that establishes connections with other nerve cells). These are generated about two weeks into a mouse's embryonic development in a specific area of the early brain. To get a source of these GABA cells before they matured, the researchers simply dissected out that part of the embryonic brain. To make sure they could find these cells in the adult animals, the mice were genetically tagged with a gene that makes a fluorescent protein.
Returning to the epileptic mice, the authors created three groups: untreated mice, mice in which the immature neurons were injected into the relevant region of the brain (the hippocampus), and mice in which the cells were injected into an irrelevant part of the brain (the amygdala).
Sixty days later, the cells that glowed green (meaning they came from the transplant) had matured and integrated into the adult brain. A number had migrated away from the site of injection before maturing so that they were more widespread in the brain rather than simply clustered at the injection site.
The procedure was largely a success. Seizures were reduced by more than 90 percent in the animals with the appropriate injections (compared to either of the control groups). Half the mice didn't experience any seizures for the week that they were monitored. In addition, the treatment blocked another of additional symptoms: the mice were less aggressive, less hyperactive, and showed better spatial memory.
But you shouldn't think of this as reversing the pilocarpine treatment. The structural changes that occur within the brain in response to the drug were still present. The creation of new inhibitory cells in the hippocampus didn't reverse all the symptoms; the mice were still prone to experience anxiety and appeared hyperactive when placed in a stressful situation. Plus, for some reason, injecting the immature neurons into the wrong location—the amygdala—successfully blocked hyperactive behavior.
Rather than reversing the impact of the drug treatment, the added inhibitory neurons blocked them from triggering epilepsy. This is potentially more valuable given that epilepsy in humans has a variety of causes.
But it's important to emphasize that this work is just a first step toward a treatment (although a valuable one). The obvious follow-up step would be to generate the immature neurons from stem cells. That would involve first forcing the cells to adopt a neural cell fate, then getting them to adopt the identity of the region that produces GABA inhibitory neurons. The procedure should then probably be tested on other models of epilepsy to make sure the effect is general. All of these validations will be essential before it makes sense to try this procedure in humans.
Nevertheless, this was an important first step—and a very nice piece of research.
Nature Neuroscience, 2013. DOI: 10.1038/nn.3392 (About DOIs).
reader comments
26